Do you consider fitting a patient in a scleral lens each day, and if not, why not?
The history and evolution of scleral lenses is quite interesting. The conceptualization of such a visual device occurred long before the actual advent of the scleral lens. Once the device was a reality, the first scleral lenses had many limitations that resulted in the extinction of the product. Technology and advancements have allowed for the reemergence of the scleral lens. The usage of the modality has steadily grown over the past 10+ years. Today’s scleral lens is very different than yesterday’s lens and this article will explore the evolution of the design and its application over the past few years. Do you consider fitting a patient in a scleral lens each day, and if not, why not?
The Traditional Thought
Who should wear scleral lenses? The traditional thought has been that scleral lenses are the lens to go to when nothing else works. Many contact lens professionals only reach for scleral lenses for patients with irregular corneas such as keratoconus, pellucid marginal degeneration, post-surgical, post-trauma or ocular surface diseased. Without a doubt, these patients have benefitted, and will continue to benefit tremendously with scleral lens designs.
Why are scleral lenses so successful for these difficult-to-fit patients? The most obvious answer is that the lenses are able to be stabilized on an irregular surface that no other design will fit. They completely vault the irregular surface of the cornea and land on the more regular surface of the sclera. But what are the other reasons that make this design successful?
• Comfort: Scleral lenses offer unbelievable comfort to the wearer. The large design stays tucked beneath the lids and moves very little. If you were to manufacture a soft lens in an intralimbal design (a diameter that stays inside of the margins of the limbus, usually 11 millimeters or smaller), the wearer would be aware of the edges and would not find it very comfortable to wear. The rigidity of the material has less to do with the comfort than the size and design of the lens.
• Stability: Scleral lenses are very stable on the eye offering consistent stable optics. The lens is unlikely to decenter or to dislodge from the eye during eye movement or activity. This provides many benefits for not only your everyday contact lens wearer, but especially for active contact lens wearers.
• Consistent Vision: Scleral lenses are fit with a tear film between the cornea and the back surface of the contact lens. The cornea remains consistently moist providing vision that does not fluctuate or deteriorate due to dryness. Soft lenses are dependent upon consistent moisture to offer the best optics. The moisture level maintained by the lens can vary based on environmental conditions, medications or patients who just do not produce a sufficient volume or quality of tears. Those patients with the ideal tear film would likely find scleral lenses and soft lenses equally comfortable with similar visual quality. Those without this ideal tear film may find a scleral lens preferable for all day comfort and visual performance. A study that seems to confirm this thought will be presented in this article.
• Reduced Glare and Starbursts: Scleral lenses have very large optic zones that stay centered over the pupil allowing the patient optics without flare and glare. Traditional corneal lenses have smaller optic zones and move quite a bit on the blink which sometimes allows for the peripheral curves to move into the visual axis creating light reflections and starbursts. The larger optical zone is beneficial to everyone, but especially to athletes, patients with large pupils and patients who experience flare and glare at night when the pupils dilate.
• Reduced Dryness: Scleral lenses are fit with a tear layer between the cornea and lens that stays consistent throughout the day. The consistent tear film keeps the surface of the cornea lubricated and allows for the scleral lens to be worn comfortably from the moment of application until the lens is removed. As a person with dry eyes, I have tried every modality available and find my wearing time to be the best with scleral lenses.
With all of these benefits, why only offer these lenses to patients as a last option? Wouldn’t it make more sense to consider scleral lenses as a potential option for every patient who comes to you to be fit for contact lenses?
Fitting Characteristics
Rigid lenses are known for crisp, stable optics but are often overlooked due to poor comfort. The general perception is that the discomfort is due to the “hard” material of the lenses. The reality is that it is the lens design that factors more into the comfort of the lens than the material itself. A 9-10 millimeter diameter soft lens would not be a comfortable design to wear just as a small corneal lens is not comfortable initially and requires a period of adaptation.
When first learning to fit lenses, we were taught that rigid lenses were intralimbal, while soft lenses were extralimbal. Intralimbal means that the lens is designed to fit within the margins of the limbus – the entire fit is on the cornea. An extralimbal design fits beyond the margin of the limbus and is fit either to the sclera alone, or is fit to both cornea and sclera. The edges of a lens fit in this manner will stay tucked beneath the eyelids and will not move much on the blink thus causing little to no mechanical awareness of the lens in the eye. Soft and rigid lenses alike will provide comfort due to the extralimbal design, and some find rigid lenses even more comfortable as the lens does not dehydrate and create fluctuations in vision and/or comfort during wear.
A properly fit scleral lens will not touch the cornea at all, will provide clearance at the limbus and will land tangent to the conjunctival tissue covering the sclera. The lens will settle into the soft conjunctival tissue with wear time. The majority of the lens settling will occur in the first 30 to 60 minutes, but the lens can continue to settle more over the first few weeks of wear. The larger the lens, the more the mass and the more settling will occur. Because of this, larger scleral lenses must start with more clearance over the cornea than smaller scleral lens designs.
![Figure 1. Predicting estimate of oxygen transmissibility of scleral lenses. [Contact Lens and Anterior Eye 35(2012)266-271.] This graph shows that a thinner lens with a higher Dk will allow more oxygen to pass through to the cornea.](/wp-content/uploads/2016/01/Benefits-Figure1.jpg)
Figure 1. Predicting estimate of
oxygen transmissibility of scleral lenses. [Contact Lens and Anterior
Eye 35(2012)266-271.] This graph shows that a thinner lens with a higher Dk will allow more oxygen to pass through to the cornea.
Larger Designs vs. Smaller Designs
Large diameter scleral lenses are generally 15.5 millimeters or larger and require a minimum of 250 to 350 microns of central clearance. Smaller diameter scleral lenses tend to range in diameters of 14 to 15.5 millimeters and require less than 350 microns of clearance, usually in the range of 175 to 200 microns.
Why is this important?
A point of significance is that the thickness of the tear layer will impact the amount of oxygen that is transmitted to the cornea. Several studies have proven that it is much healthier to fit a thinner scleral lens (350 microns or less) with a central clearance as close to 200 microns as possible. Some of these studies are Michaud et al, 2012 (Figure 1) which used a theoretical model showing the impact of oxygen delivery on the cornea at various lens and tear thicknesses; Compañ et al, 2014 also using a theoretical model to show the signs of induced hypoxia after several hours of wear with thick, highly vaulted scleral lenses; and Jaynes el al, 2015 which used a theoretical model to show that the corneal consumption of oxygen is higher after wearing scleral lenses exceeding the thickness and vault values considered safe by the two prior mentioned studies.
Patrick Caroline, FAAO presented at Global Specialty Lens Symposium in Las Vegas in January 2015 that the level of edema that is present during the wear of scleral lenses is clinically insignificant as it is approximately 2-3%.
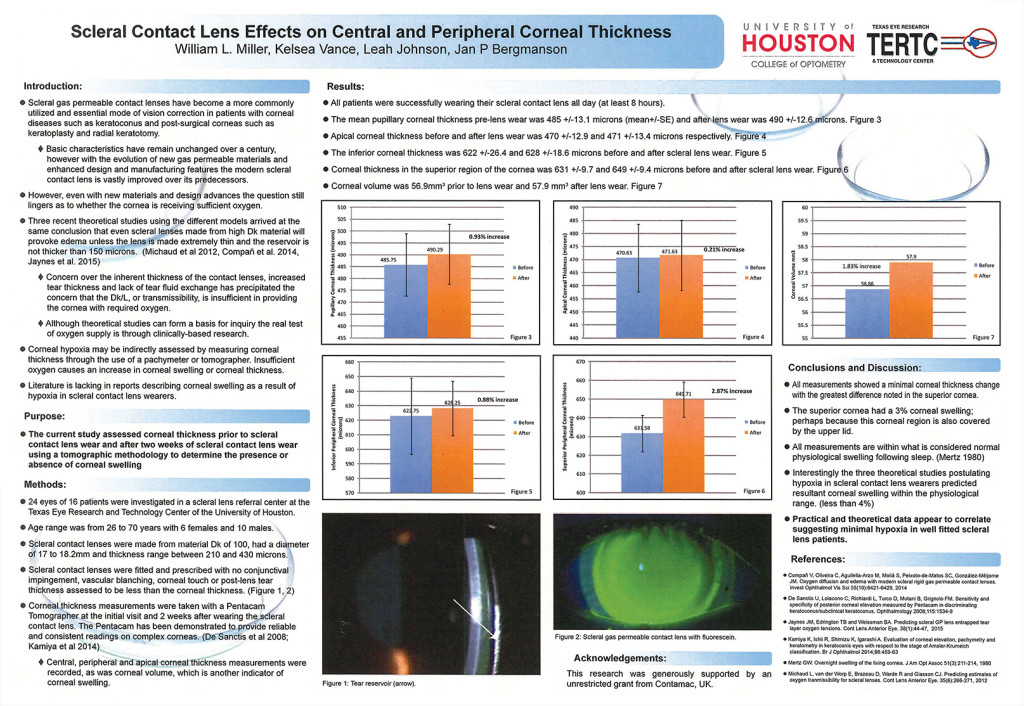
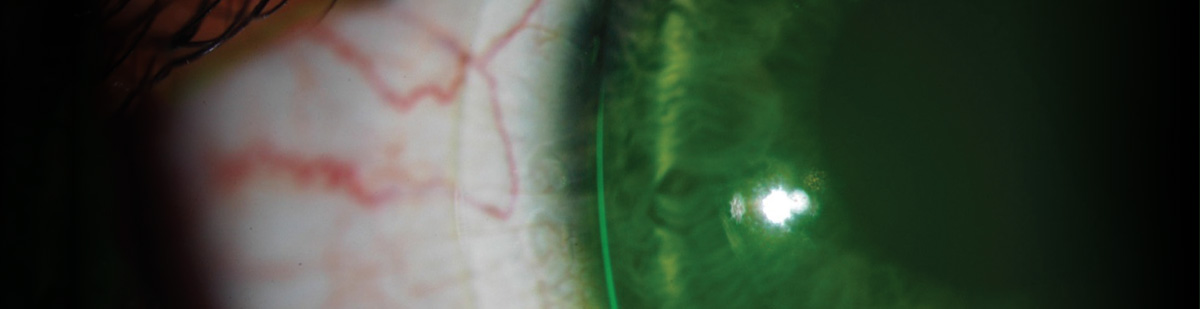
Figure 2
This value is similar to the edema present upon awakening in the morning, or equal to the amount of edema caused when the eyes are closed for a significant period of time. A poster presented at ARVO this year by Miller, Vance, Johnson and Bergmanson (Figure 2) demonstrates the results of a study performed on patients wearing scleral lenses between 17 and 18.2 millimeters of diameter with approximately 400 microns of clearance. The participants wearing these larger diameter scleral lenses experienced corneal swelling with the most significant edema in the superior cornea (approximately 3%). It is hypothesized that the swelling was greatest in this area as the result of the upper lid, which in most patients will cover the most superior part of the cornea in addition to the lens during wear. Scleral lens wearers have very little time that the cornea is not in a state of chronic low-level hypoxia, between the hypoxia that exists in the closed lid state and that which exists during scleral lens wear.
There is no question that when evaluating the risk-versus-benefit value for a patient with an irregular cornea, that the benefit of the lenses in most instances outweighs the potential risks.
What about normal corneas? When fitting normal corneas, a minimalist approach will offer the maximum benefit with the least amount of risks. Fit the lens with the least diameter, least lens thickness and least amount of central vault that you can. Seek out a design that offers a vault approximately 200 microns centrally and decreases over the limbus to 30 to 60 microns.
Minimal clearance over the limbus will offer maximum oxygen to the stem cells that live there. By fitting a design with this tear profile, you will create a tear film that helps support the weight of the lens while also providing sufficient oxygen to the cornea. Though you want limited clearance over the limbus, clearance is absolutely necessary to avoid impacting stem cells (DeNayer, 2015 and Bath et al, 2013). (Figure 3 and Figure 4)
Figure 3 shows an optic section being used to evaluate and measure tear film clearance on a smaller mini-scleral lens. The thickness of the contact lens is 280 microns and in comparison, the tear film is approximately 150 microns. Figure 4 depicts an appropriate diameter on a normal eye, usually around 14.9 millimeters. Photo Courtesy to Blanchard Contact Lens, Inc.
Another factor to consider when choosing the appropriate scleral lens is handling. Scleral lens fitters often tell me that the reason that a patient failed at scleral lenses was simply the inability to handle the lenses. A patient with an irregular cornea who can only achieve optimal vision through a scleral lens will be highly motivated to learn the skills necessary to wear the design. A patient with a normal cornea may have less motivation. Smaller scleral lens designs often work well for normal cornea patients as they are similar in diameter to soft lens designs that the patient may already be accustomed to handling.
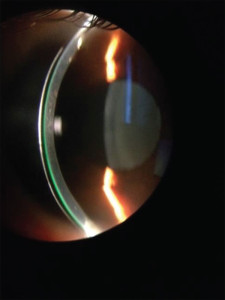
Figure 3. shows an optic section being used to evaluate and measure contact
tear film clearance on a smaller mini-scleral lens. The thickness of the contact lens is 280 microns and in comparison, the tear film is approximately 150 microns.
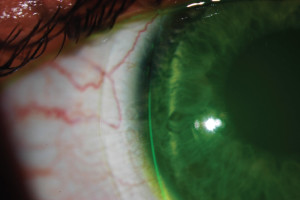
Figure 4. depicts an appropriate diameter on a normal eye, usually around 14.9 millimeters. Photo Courtesy to Blanchard Contact Lens, Inc.
Patients You See Every Day Who Could Benefit From Scleral Lenses
Contact lens practices serve patients every day that could benefit from the advantages of scleral lenses. This modality should be offered as an option to any patient who may benefit, rather than just considered only when nothing else works. As with any contact lens modality, once you learn the nuances of fitting the design, it is no more difficult to master than any other product offering. Take the time to invest in yourself and partner with your gas permeable laboratory so that you can offer the option to any patient who may benefit.
End of Day Dryness/Reduced Wear Time: A common complaint of soft contact lens wearers is that the lenses dry out during the day and that wearing time is affected. End of day dryness can lead to poor vision and comfort that ultimately causes the patient to drop out of contact lens wear entirely. John Rumpakis, O.D, M.B.A published an article in January 2010 in Review of Optometry, New Data on Contact Lens Dropouts: An International Perspective stating that more than one in six of your contact lens patients will discontinue contact lens wear. The economic impact to the practice of one contact lens dropout over a lifetime can be as much as $24,000. According to the data in this article, approximately 50% of the people surveyed in the U.S. stated the biggest reason for discontinuing contact lens wear was discomfort.
Many contact lens practitioners will try different soft lens materials and designs in an effort to improve comfort and wear time.
Practitioners will also change solutions, including solutions with various lubricants or without preservatives, or recommend additional lubrication drops during wear. For many patients, a balance can be found that offers acceptable wear of the lenses, but a percentage drop out of wear because comfort cannot be found or the regimen required is not worth it.
Scleral lenses offer these patients an opportunity to wear lenses with improved comfort and for longer wearing schedules. Scleral lenses maintain a fluid layer behind the lens and against the cornea during all wearing hours. This tear layer keeps the cornea bathed in moisture all day providing relief from dry eye symptoms. Scleral lens patients experience crisp, clear vision with lenses that offer consistent comfort from the time they apply them in the morning until they remove them in the evening.
Athletes: Athletes have demanding visual needs. It is critical that an athlete have stable, crisp and consistent vision delivered by a secure, comfortable visual device that will allow for performance at its highest level with the least amount of distraction. Complications faced by athletes with contacts are that the vision may vary during activity due to dehydration or rotation if wearing a sphero-cylindrical correction, the lenses may dislodge or pop out during activity, or debris may get behind the lens causing discomfort and visual disturbances.
Scleral lenses offer many benefits for patients who live active lifestyles or who are athletes. The lens fits very securely to the eye exhibiting little movement.
The lens is highly unlikely to pop out, dislodge or allow debris behind the lens. The lens maintains a consistent tear film between the corneal surface and the back of the lens offering clear, consistent and stable vision. The vision will not fluctuate due to lens movement, rotation or dehydration. Scleral lenses have large optical zones which allow the athlete a large field of view without flare or glare that they may experience when the peripheral curves of smaller gas permeable (GP) lenses cross into their visual axis. The lens is safe to wear during physical activity and in some cases may even provide protection from trauma (Altman, 2012).
Unhappy Soft Toric Lens Wearers: Some soft toric contact lens wearers tolerate less than optimal vision because they are unable to, or don’t want to wear corneal gas permeable (GP) contact lenses. They accept vision that is not as good as their eyeglasses, usually due to lens dryness or lens instability causing a fluctuation in vision. In many cases, scleral lenses can offer these patients the crisp, stable vision of a GP lens with the comfort of a soft lens.
A poster at the American Academy of Optometry in 2012 showed the results of a clinical study comparing soft toric contact lenses to small scleral lenses. The study was Clinical Evaluation of a Large Diameter RGP Lens for the Correction of Refractive Astigmatism (L. Michaud, S. Woo, A. Dinardo-Lotoczky, J. Harthan, B. Morgan, E. Bennett and R. Reeder). The purpose of the study was to validate the comfort of a large diameter GP scleral lens. Patients who were current happy soft toric lens wearers were the participants of the study.
The study was a multi-center, cross-over, randomized study. All patients were fit in the same soft toric contact lens (Biofinity® Toric by CooperVision®), regardless of their 20habitual contact lens. All patients were fit with the same large diameter GP scleral lens (Onefit™ by Blanchard Contact Lens, Inc.). Half of the patients wore the soft lens option first, while the other half wore the large diameter GP scleral lens first. The patients switched modalities half-way through the study. Thirty-six patients completed the study, 25 female and 11 male. The result was that there was no statistical difference in comfort or performance during day-to-day tasks and in a forced choice, 52% chose to stay with the large diameter GP scleral lenses over soft lenses. This is a pretty amazing statistic considering the study used HAPPY soft toric patients. Imagine how much larger that percentage may have been if the study patients were unhappy soft toric patients!
Presbyopic Patients: A presbyopic patient has to cope with visual compromise regardless of the visual system, but the compromises experienced while wearing contact lenses can be particularly frustrating. A presbyopic patient with astigmatism that exceeds 0.75D of corneal cylinder often finds it challenging to find a contact lens that gives consistent and crisp vision at both near and distance. These patients frequently experience a reduced or compromised tear film that is unable to support stable vision through a soft toric lens and many cannot or prefer not to adapt to GP lenses.
Scleral lenses with multifocal correction can offer a solution to this demographic.
The design in scleral lenses is typically a center near, as the lens does not move enough to translate between near and distance vision. The patient experiences simultaneous vision, providing near, intermediate and distance vision to the retina all at once and the brain learns to pay attention only to the clear light rays at any given distance. Ten to fifteen percent of the population has difficulty adjusting to simultaneous vision, but that leaves 85-90% of presbyopic patients that you care for that can benefit from scleral multifocal lenses. Personal experience with the design has proven to me that it is comfortable to wear and provides excellent vision at all distances.
Post-LASIK Surgery Patients: Some may categorize these patients as being irregular cornea, but many of these patients have fairly regular corneas with the exception of the flattened central area. A patient who has had this procedure may find that they are left with a mild prescription that they cannot or choose not to have enhanced with additional surgery or they may have had the procedure some time ago and are now presbyopic. Scleral lenses with an oblate design can be very beneficial to these post-surgical patients. The oblate lens incorporates reverse geometry creating a lens that is flatter in the center than in the periphery so that it mimics the surgically altered cornea. This oblate design creates a more uniform tear layer optimizing fit and oxygen transmissibility.
Post-LASIK patients do not always do well with soft lenses after surgery for two reasons. First, post-surgical patients often suffer with dry eyes and they may not have the quantity or quality of tears to provide the moisture necessary to support the soft lens. Secondly, a soft lens will drape the shape of the oblate cornea rather than hold its shape. The instability of the material does a poor job of delivering crisp optics.
Scleral lenses will offer these post-surgical patients the vision of a GP with the comfort of a soft lens. The ability to wear these lenses intermittently, unlike corneal GP lenses, also provides a flexibility that a post-refractive surgery patient may enjoy as they may find that they only require better vision for specific tasks. The oblate scleral lens is also available with presbyopic correction.
You may ask, since we are vaulting the entire cornea and fitting the sclera, why does it matter if the design is oblate to match the corneal shape? This is an excellent question and the explanation is that the oblate design allows for optimal oxygen delivery to the cornea by reducing excessive clearance over the surgically altered surface (refer to the earlier Michaud et al, 2012 study) as well as optimizing vision. A patient attempting to view through a very thick tear layer may experience reduced contrast sensitivity and a reduction in best visual acuity.

flexibilFigure
5. Injury of a mini-scleral wearer. This photo was published in Contact Lens Today, Sunday January 20, 2014. The patient was wearing a small mini-scleral lens for normal eyes while playing basketball. The lens protected the cornea when the wearer was poked in the eye and as a result, the only injury suffered was a subconjunctival hemorrhage as the fingernail slipped passed the diameter of the lens and scraped the conjunctiva.
Enhanced Designs
Scleral lenses are available with enhanced design features to improve vision and comfort. Toric peripheral curves are available to improve the alignment with the conjunctiva and to improve centration of the lens. It is rare to need toric peripheral curves on scleral lenses 15 millimeters or smaller (Van der Worp, 2014), but the conjunctiva is often much more toric in nature further out in the periphery. Scleral lenses are also available with anterior toric optics. Anterior toric optics will correct residual cylinder should there be any. The large design of the toric, often combined with some strategically placed prism, will keep the lens on axis and stable. Troubleshooting the orientation of an anterior toric scleral lens is similar to and follows many of the rules of troubleshooting a soft toric lens, with one exception – dryness is rarely the cause of poor vision!
Benefits to Your Practice
Scleral lenses will help you differentiate yourself to your patient by allowing you to offer a product that is healthy, comfortable, provides excellent vision and utilizes the latest technology, materials and designs. After your initial investment in yourself to learn the skills necessary to fit the lens, you can fit scleral lenses on patients with normal corneas efficiently, effectively and profitably. When you compare the annual cost of frequently replaced soft lenses to that of the annual cost of scleral lenses, the cost is similar to the patient but the profit margin to your practice is usually much higher with scleral lenses. The ability to offer your patient an industry leading product that offers health and vision benefits while improving your bottom line is a winning scenario for you and your patient alike.
If Not, Why Not ?
Do you offer scleral lenses to at least one patient you fit in contact lenses each day? If not, why not? As the previously mentioned studies have shown, scleral lenses fit with a minimalist approach (minimal lens thickness, minimal tear film, especially over the limbus, with a minimal diameter) offer a healthy option for your patient. Added benefits are all day comfort with consistent, stable vision. If you do not offer your patients leading edge products, your competition will! Invest in yourself, partner with your scleral lens laboratory and start offering scleral lenses to patients who could benefit today!
Clinical Pearls : Overcoming Concerns of Potential Scleral Lens Patients
Why are some patients hesitant to wear scleral lenses and how do I overcome the barriers they present? Your ability to recommend scleral lenses when you believe they are the best choice, and your skill in confidently overcoming patient concerns will be a big determinant of your success with the modality.
Patient: They cost too much!
My response: I would show them the cost of a two year supply of soft lenses versus one pair of scleral lenses. The cost is usually very similar. Combined with the advantages of the design responsible for my recommendation, the scleral lens provides excellent value to the patient.
Patient: They are difficult to handle!
My response: If a current CL wearer, I remind them how difficult it was to learn to wear lenses when they first became a wearer. If new to contacts, I relate it to a new skill such as driving or a sport. I tell the patient everything has a learning curve, but I feel the advantages of this modality are worth the effort required by you to be successful. Remember to be patient and a good coach should they decide to take the challenge!
Patient: Aren’t they hard lenses?
My response: I avoid using the word “hard” lenses while still being honest. I describe the lenses to the patient as oxygen permeable lenses with leading edge technology that combines the best attributes of soft lenses (comfort) and rigid lenses (vision). Offer the patient a chance to experience the feel of a diagnostic lens with no obligation. Choose your diagnostic lens wisely making sure you do not put a lens on that is too flat. You may spend an extra 5-10 minutes of chair time, but once the patient experiences the comfort, they are often convinced.

Ledonna Buckner is a Virginia Licensed Dispensing Optician specializing in unusual contact lens fitting cases. She is a Certified Ophthalmic Assistant, Fellow of the Contact Lens Society of America, past Board of Director for the CLSA and past Editor-in-Chief for EyeWitness Magazine. She has extensive experience as a speaker on contact lens subjects across the USA. Presently, Ledonna is the Senior Account Manager, Mid-Atlantic Region for Blanchard Contact Lenses and is responsible for day to day account management, account education and training and technical fitting consultation.


